With the start of 2025, the Healthcare landscape is changing more rapidly and frequently. HIPAA compliance is the center of consideration in every health sector. Compliance with HIPAA is critical because the U.S. Department of Health and Human Services (HSS) Office for Civil Rights(OCR) is struggling because of the 22 penalties for violating HIPAA.
HIPAA compliance is beyond the legal requirement. It’s crucial to follow for the patient’s sake and organizational integrity.
Health Insurance Probability and Accountability Act is the cornerstone of patients’ privacy and security. The enforcement of the HIPAA Act has brought various challenges to the healthcare department.
Data security and privacy are not as simple as before. Technology has made it easier and more convenient to be stolen.
The data can be misused and leaked. This is why organizations, especially those with slightly more relation with the health sector, need to understand the HIPAA Act. By following this act organizations can stay compliant.
HIPAA act is crucial for patient’s security and privacy as well as protected health information.
This blog will guide you through HIPAA compliance meaning, why it’s important, and what are the elements and benefits of following this compliance.
Definition Of HIPAA Compliance
The Health Insurance Portability and Accountability Act (HIPAA) is a sequence of regulatory practices that ensure the security and privacy of health information. This act was devised in 1996. Simply this act is about obeying all the rules set by HIPAA.
This act is regulated by
- Department of Health and Human Services (HHS)
And enforced by
- Office for Civil Rights (OCR)
Three rules organizations must follow to be HIPAA compliant are
- The Privacy Rule
- The Security Rule
- The Breach Notification Rule
| “As digital healthcare data proliferates, an AIM solution paired with HIPAA compliance policies helps create a wide umbrella of protection against violations.” |
Why Is HIPAA Compliance Essential?
The main purpose of HIPAA Compliance is to keep the patient’s data confidential. The data can be in any form such as paper, oral or electronic.
HIPAA compliance is essential to follow for all health sectors because it can help in
- Protecting patient’s data and information can protect organizations from costly security breaches.
- It can protect the organization from penalties.
- It can reduce cybersecurity threats.
- It can minimize organizational vulnerabilities and reduce legal procedures.
- Staff members can frequently retrieve and update protected health information.
Who Must Comply With HIPAA?
HIPAA compliance is required for organizations. Third parties also handle or manage protected health information (PHI). HIPAA requires covered entities, business associates, subcontractors, or any other entities should be HIPAA compliant.
Entities that need to be compliant include
Health Information Exchanges (HIEs)
The organization that provides health information in facilitating patients must ensure HIPAA compliance. It protects the confidentiality and integrity of shared information.
The organization that needs to be HIPAA compliant also includes billing firms and health plan administrations. It also includes individuals like lawyers, It staff, and accountants working in health sectors.
Covered Entities
An organization or company that facilitates payment, health operations, or medical relief in a healthcare sector across different payment channels is considered a covered entity.
They can create, collect, and transmit PHI electronically.
For instance, nursing homes, health care centers, medical care entities, and health insurance providers. This can include third-party healthcare businesses as well.
Business Associates
The company that has protected health information access and supports the treatment, operation, or any operations is known as a business associate.
For instance, It providers, e-mail hosting services, electronic health record platforms, etc.
What Are HIPAA Compliance Checklist?
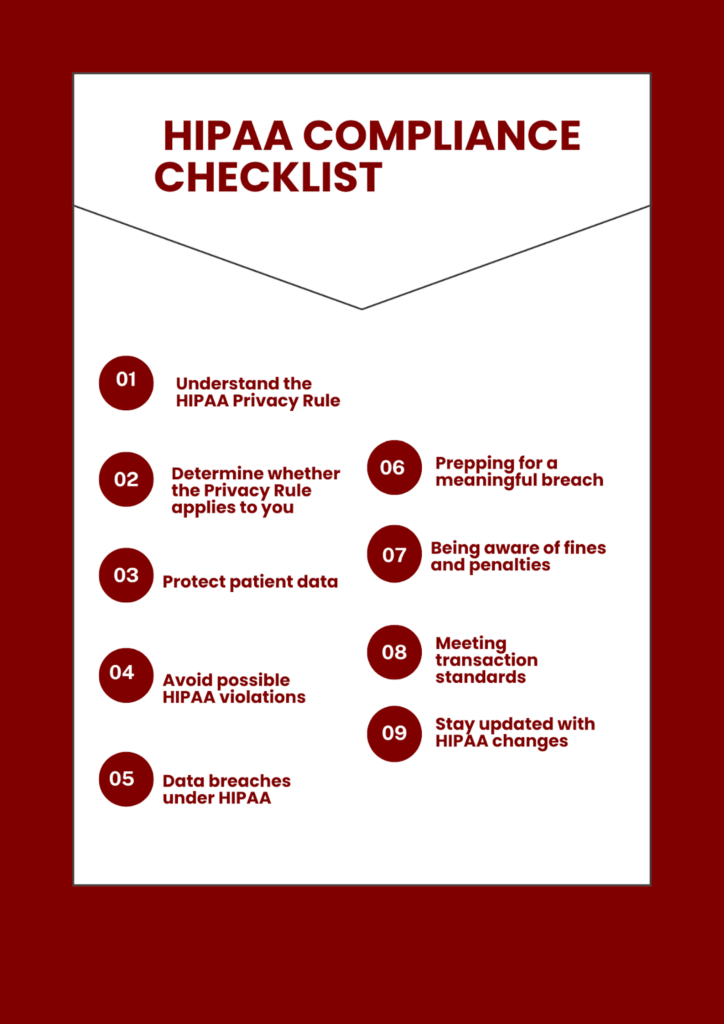
Achieving HIPAA compliance is difficult and cost-effective. Breaking it down into manageable steps can help you manage compliance more easily.
The checklist below can help you to follow the right track.
Knowing The HIPAA Privacy And Security Rules
The first and foremost step of the compliance checklist is to understand what it means to comply with HIPAA.
The total length of HIPAA rules is 115 pages according to regulations. Analyzing all of it falls into three categories
- Administrative security that protects the data security.
- Physical safeguard deals with the safety of equipment.
- Technical safety protects the technical data issues.
This can be complex to understand and implement, starting with a big frame and then breaking it down into parts that can draw details.
Determine Whether The Privacy Rule Applies To You
Privacy rules and policies define the information that is protected under the umbrella of HIPAA and by who is covered by the rule.
These entities include
- Heath plan
- Healthcare clearinghouses
- Healthcare providers involved in electronic transformation
If you are uncertain about the category you can use tools (covered Entity tool) to find out the right category.
If you fall in the covered entity these are guidelines you need to understand
- what constitutes protected health information (PHI)
- The general principle is to see how to share information.
This can help you how you can apply policy rules to you.
Protection Of Patient Data
All information is not protected under HIPAA, there are permitted uses of PHI are available without authorization.
For example, patient data can be anonymized. To achieve HIPAA you need to identify the patient and patient’s information for whom you want to protect the data.
After that, you analyze what data falls under HIPAA regulations.
Avoid Possible Hipaa Violations
To avoid HIPAA violations you need to do a risk assessment. You can address the gaps, security issues, and implementation of compliance. HIPAA compliance software controls include
- Data Encrypting
- Proper working of devices or documents
- Conducting cybersecurity training
- conducting compliance requirements
- Accessing patient records without need
- Disposing of PHI with security
- Business associates sign a contract agreeing to HIPAA compliance
- Implementing system monitoring for access control
Data Breaches Under HIPAA
Data breaches under HIPAA can include
- unauthorized possession
- release of protected health information
- Unauthorized access to HIPAA data compliance and information
- Information that can risk the patient’s life.
To secure and prevent all the breaches proper security measures are needed. The security of internal and external measures should be ensured. It needs proper training of staff as well as the teaching programs of cybersecurity programs.
Prepping For A Meaningful Breach
Breaches can affect more than 500 individuals under a single jurisdiction. They can be reported to HSS OCR within 60 days after the discovery of the breach. Breach-infected individuals should be informed. Law enforcement should inform agencies too to alert the pointed people.
Being Aware Of Fines And Penalties
OCR resolves HIPAA violations through non-punitive methods like voluntary compliance or offering technical guidance. It assists covered entities with non-compliant areas.
Meeting Transaction Standards
HIPAA calls for all data transactions or conveyance to meet the Data Exchange Standard. Some of the common transactions include:
- Progress of status
- adjustments of benefits
- Payment and settlement advice
- Adequacy
- Authorizations
Stay Updated With HIPAA Changes
HIPAA compliance is an ongoing process. staying up-to-date with the latest developments is important. The updated HIPAA rules include
- Examination of patients’ PHI with notes and photographs.
- Maximum time of providing PHI access for 15 to 30 days.
- Entities should schedule fees for PHI on their websites.
What Are HIPAA Compliance Requirements?
HIPAA regulation outlines a set of national standards that all covered entities and business associates must address.
HIPAA regulations shape a set of national standards and policies that cover all entities. The entities and business associates address these standards. HIPAA compliance requirements include
Security Rule Requirements
Security rule requirement protects and safeguard the patient’s PHI with confidentiality and integrity. The requirements can be electric.
For this organizations need to analyze and cater to the security risks with appropriate security policies to ensure the compliance workforce.
Security rule shapes the guidelines into three sections.
- Administrative safeguards
- Physical safeguard
- Technical safeguard
Administrative safeguards include policies, actions, and procedures involved in protecting PHI.
Technical safeguard includes the technology that is associated with PHI while physical safeguard includes the building and workstation security.
Privacy Rule Requirements
Covered entities need to follow the rules to comply with privacy rules which include
- Notify patients about their privacy rights.
- How the organization will use their information.
- How to Adopt privacy procedures
- Training of employees to follow procedures.
- Assignment of a HIPAA compliance officer
- protecting patient records containing PHI.
Privacy rule is a least needed requirement.
This is established on the principle of PHI and shouldn’t be disclosed till the job is done. This requirement protects the health information of the patient with confidentiality.
| “HIPAA beholden entities must have proper safeguards in place to keep PHI secure.” |
What Are The Elements Of Effective Compliance
There are seven effective compliance elements advised by the HHS Office of Inspector General (OIG). Organizations also devise their compliance programs. As these are minimum requirements for effective compliance. Effective compliance programs must handle all the seven elements which include.
- Implementing written policies and procedures
- Designating a compliance officer
- Conducting effective training
- Developing effective lines of communication
- Managing internal monitoring and auditing
- Enforcing standards with disciplinary guidelines
- Responding promptly to detected problems for active action
Implementing Written Policies And Procedures
The foundation of the compliance program is based on the policies and procedures you follow.
The procedures include
- A detailed compliance program
- Ethics and code of conduct
- Training of employees with an action plan
- A detailed recovery plan
The policies and procedures for HIPAA compliance solutions need certain requirements. The requirements include the behaviors, actions, and day-to-day run of all rules to stay compliant.
This requires an outline to maintain the workforce to action in violation of compliance.
Proper training of employees and staff members is necessary to train with the written policies and up-to-date regulations. Employees can be provided with HIPAA compliance certification to know how many employees can deal best.
Designating A Compliance Officer
Policies implementation in an organization and adherence to them leads to gaps in compliance.
Violation of compliance puts organizations at risk. It can also add penalties to an organization.
To make the policies work organization should appoint a compliant officer. The compliance officer can help in maintaining and adhering to the policies and procedures. The compliance officer will monitor and advise the compliance plans.
Conducting Effective HIPAA Compliance Training
Compliance programs are ineffective without awareness. It is important to educate and train the employees for effective results of the policies and procedures.
Training programs can include
- How to train new employees?
- Who will be responsible for the training?
- What type of training and information should be given to employees?
- Who will ensure the compliance management training?
The Training Program Is An Ongoing Process. Training Should Be Regular Because It Can Help Employees Stay Up-To-Date With Comply With Policed And Procedures.
Developing Effective Lines Of Communication
Open communication is crucial to maintaining transparency. Organizations can solve problems, provide feedback, and help when needed.
Only clear communication channels can help in maintaining a transparent culture. It is essential to ensure the customer their information is in the right place.
Clear communication policies, honest feedback, and surveys can be a great help.
Managing Internal Monitoring And Auditing
Achieving compliance isn’t an end. It is an evolving process. Continuous monitoring and adherence is a success.
Internal HIPAA compliance audits, external audits, compliance inspections, and continuous reviews can help organizations identify the key risks and end up with solutions.
Enforcing Standards With Disciplinary Guidelines
How will HIPAA standards be enforced in the organization? Enforcement is an important element of compliance. It helps people to understand the risks and the seriousness of the violations. It helps in steps to avoid them. Clear disciplinary guidelines keep compliance consistent.
Best policy management systems support initiatives by notifying employees about the new policies and regulations to stay compliant.
Responding Promptly To Detected Problems For Active Action
Mitigating the risks quickly and effectively lessen the harm and increase the scope of productivity.
Organizations need to create an action plan to address the potential risks with the contributed results in avoiding them. The plan should mention the notification clarification. It will be valuable to call the specific resource for a particular risk management.
What Are Common HIPAA Violations?
Few most common causes of HIPAA violations and fines can include
- Stolen digital devices
- Stolen USB device
- Malware Incident/ Virus Attack
- Hacking
- Business associate breach
- EHR breach
- Office break-in
- Sending PHI to the wrong patient
- Discussing PHI outside of the office
- Social media posts
These HIPAA violations commonly fall into different categories which are
- Use and disclosure
- Improper HIPAA security compliance safeguards
- The Minimum Necessary Rule
- Access controls
- Notice of Privacy Practices
Final Thoughts
As we look forward to 2025, HIPAA compliance services remain important in healthcare data protection. Technologies are ever-evolving to meet new challenges in the digital age. The importance of HIPAA compliance cannot be ignored. It protects patient privacy and safeguards healthcare organizations from heavy penalties and reputational harm. The elements and requirements of HIPAA compliance must adhere to stay successful in the frequently changing world.
FAQs
What is Hipaa?
HIPAA (Health Insurance Portability and Accountability Act) is a set of standards for healthcare providers, insurers, and related entities. It ensures the privacy and security of medical records and patient’s health data.
How To Comply With HIPAA Privacy Rules?
To comply with the HIPAA Privacy Rule, healthcare providers and covered entities must implement and safeguard patients’ protected health information (PHI). which include
- Obtaining patient consent before sharing PHI
- Providing access to medical records
- Establishing policies for data handling
- Training staff on privacy policies
- Using secure communication methods for PHI access
Is It Mandatory To Follow All HIPAA Rules?
HIPAA is a regulatory requirement. All healthcare organizations and entities must follow HIPAA rules without exception. Violation of any rule can lead to heavy fines and legal penalties.
Also Read: HIPAA Certification: What It Covers And Who Needs It













+ There are no comments
Add yours